Vital Perspective
Confronting the Global Cancer Crisis
How Brazil’s Response to Noncommunicable Diseases Can Guide a Global Prevention Strategy
It’s morning in Sao Paulo, Brazil.
Like clockwork, rush hour traffic floods the streets and subways with a frenzy of people, scooters, cars, motorcycles—and the unmistakable crinkle of packaged snacks.
Widely available and hard to resist, snacks like chips, cheese puffs, and sugary drinks are a frequent quick fix for busy Brazilians. These treats—all falling under the umbrella of ultra-processed foods—are cheap, tasty, and often a practical choice to replace fresh meals for the poor or time-poor consumer.
But their convenience comes with a deadly cost. Industrially manufactured to appeal to consumers, ultra-processed foods are laden with added sugars and chemical additives. They’ve become a dietary staple in Brazil, and as consumption of unhealthy foods and obesity has increased, so too has the risk of cancers linked to these products.
However, unhealthy diets are only one part of the picture. Other major risk factors—like tobacco use, alcohol consumption, air pollution and physical inactivity—have also fueled Brazil’s growing cancer burden, making it the country’s second leading cause of death in 2019.
One in five Brazilian deaths were caused by cancer in 2019.
Percent of Total Deaths by Region, Brazil, 2019
Global Burden of Disease Collaborative Network. (2022). Global Burden of Disease Study 2021 (GBD 2021) results. Institute for Health Metrics and Evaluation (IHME). https://vizhub.healthdata.org/gbd-results/
Global Shifts
Noncommunicable Diseases are the World’s Leading Killers
Cancer is becoming a growing concern far beyond Brazil. Around the world, the burden of disease has shifted from infectious to chronic, noncommunicable illnesses.
Over the past century, noncommunicable diseases (NCDs) like heart disease, diabetes, chronic respiratory diseases, and cancer have overtaken infectious diseases, such as tuberculosis and malaria, as the leading causes of death and disability. This shift—known as the epidemiological transition—is closely tied to economic and environmental factors such as industrialization, improved living conditions, and longer life spans. Today, NCDs are a major global health challenge.
Noncommunicable diseases now account for 75% of non-pandemic global deaths
Causes of Death 1980 - 2021
Global Burden of Disease Collaborative Network. (2022). Global Burden of Disease Study 2021 (GBD 2021) Results. Institute for Health Metrics and Evaluation (IHME). https://vizhub.healthdata.org/gbd-results/
Among the many NCDs driving this shift, cancer has emerged as one of the most urgent and alarming threats, accounting for one in six deaths globally. The disease imposes immense social, emotional, and economic burdens worldwide, straining families and overwhelming health systems.
In 2022, cancer care in Brazil cost the public health system 3.9 billion reais (about USD $722M). This figure, which doesn’t include private health spending, is set to surge as cancer incidence is projected to rise 68% over the next 20 years, with almost one million new cases in 2040 alone. The burden extends well beyond the health care system, rippling through communities and entire generations. Beyond direct medical costs, cancer disrupts lives in ways that are harder to quantify—pulling caregivers out of the workforce, driving families into debt, and deepening social inequities. On average, caregivers spend between 30-40 hours a week caring for loved ones battling cancer, with many facing loss of employment or increased household debt due to these demanding responsibilities.
In 2021, NCDs were responsible for over
43 million deaths
presenting a global health challenge
This rising toll is complex and staggering. The risk factors linked to cancer are deeply intertwined with how and where people live, work, eat, and age. Thus, this challenge demands a strategic, multi-layered response. Many groups across Brazil, including Vital Strategies, are supporting a comprehensive approach to confront the preventable causes driving this growing cancer crisis. These efforts offer a model that other countries can look to in their own efforts to reduce cancer risk.
The Cancer Problem
The Forces Behind Cancer
Addressing cancer begins with understanding its causes. Research shows that nearly half of cancer deaths are linked to modifiable risk factors, such as diets high in ultra-processed food and sugary drinks, tobacco use, alcohol consumption, air pollution, and physical inactivity.
Exposure to these factors can trigger metabolic and physiological changes that elevate cancer risk. Therefore, identifying and targeting them is a crucial first step in reducing the burden of preventable cancers globally.
How Risk Factors Impact the Body
Risk Factors
Tobacco
Cigarette smoke contains over 80 carcinogens that damage DNA. It weakens the immune system, promotes the growth of already damaged cells, and silences tumor suppressor genes.
Read the researchRelated Cancers
Azevedo e Silva G, de Moura L, Curado MP, Gomes FdS, Otero U, Rezende LFMd, et al. (2016). The Fraction of Cancer Attributable to Ways of Life, Infections, Occupation, and Environmental Agents in Brazil in 2020. PLoS ONE 11(2): e0148761. https://doi.org/10.1371/journal.pone.0148761
These risks take root in people’s lives through a complex interplay of economic circumstances, social norms, and industry influence. Together, these factors unsuspectingly shape environments and steer consumer preferences in ways that end up driving harmful behavior.
For decades, food industry giants successfully marketed their products as healthy, time-saving solutions for the modern Brazilian household. As a result, ultra-processed products like condensed milk and instant noodles have become common staples in kitchen pantries across the country and increasingly make up larger portions of Brazilian diets. This shift, driven largely by the industrialization of food environments, has had a disastrous impact on public health, contributing to rising rates of cancer and diabetes.
Ultra-processed foods have become deeply embedded in Brazilian diets, due in part to decades of misleading marketing by the food industry.
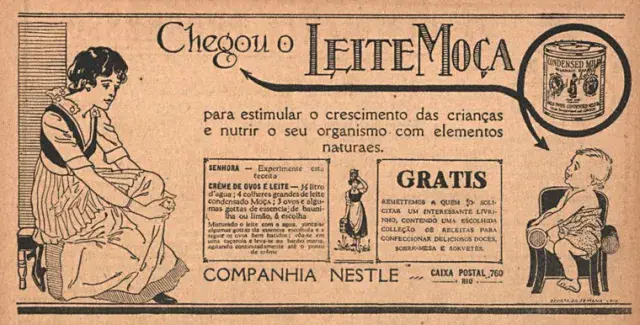
The MILKMAID Has Arrived
To stimulate children’s growth and nourish their bodies with essential elements
Nestle Condensed Milk advertisement, o joio e o trigo
Hover for translation
Political pressure has also become a major obstacle to advancing public health in Brazil. Its national anti-tobacco committee faced attacks from federal leaders with close ties to major tobacco companies. This year, the beer industry launched a parliamentary front backed by nearly 200 Congress members to advance their interests, from shaping legislation to expanding market reach. These forces operate to shape cultural habits and protect corporate interests at the expense of public health.
Tackling these challenges is tough. Ingrained cultural norms clash with health goals, while powerful industries relentlessly push harmful products and obstruct vital regulations. Government policies often falter against this resistance. This deadlock of culture, commerce, and politics ensures single fixes fail. But proven solutions do exist: smart policy can prevent needless deaths and cut cancer’s heavy economic drag on Brazil, and can serve as inspiration for the global stage.
A Playbook to Combat NCDs
In the past, the traditional public health model successfully targeted infectious diseases with interventions like vaccines, sanitation, and treatments for immediate effect. Now, as the global disease burden shifts decisively towards chronic conditions like cancer, a different approach is required.
Grounded in extensive research and experience, new strategies must promote health, protect communities, and prevent harm. Successfully tackling NCDs involves deploying interventions across policy, practices, and people to realize broad, positive public health shifts.
At Vital Strategies, we think about these interventions across three capability areas:
A History of Success
How Brazil Won the Fight Against Tobacco
While working towards change appears challenging, Brazil has already proven it’s possible. Brazil’s progress began with tobacco, the leading preventable cause of cancer, and that success has laid the foundation for broader efforts to reduce risk and improve health. Over the last 30 years, the country’s campaign against tobacco use stands as a model of coordinated action through a combination of strong laws, public education campaigns, graphic warnings, and higher tobacco taxes. This has contributed to a substantial reduction in smoking prevalence and is projected to prevent 7 million premature deaths in the next 25 years.
The timeline below highlights key milestones in Brazil’s public health response against tobacco use, including legal reforms, regulatory institutions, and national education campaigns that collectively helped drive smoking rates down.
Smoking Rates in Brazil Have Dropped by 74% Since 1989
Smoking Rates in Brazil Have Dropped by 74% Since 1989
Smoking Prevalence Among Brazilian Adults, 1989 - 2023
Ministry of Health (Brazil). (2023). Vigitel Brasil 2006–2023. https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/svsa/vigitel/vigitel-2006-2023-morbidade-referida.pdf
1989
The National Tobacco Control Program (PNCT) is created to control tobacco use and reduce nationwide smoking prevalence in Brazil
1996
Brazil enacts a national law mandating smoke-free public spaces, restricting tobacco advertising, and requiring mandatory health warnings
1999
Brazilian National Health Surveillance Agency (ANVISA) is created
2000
Brazil increases restrictions on cigarette advertisements, including banning ads in print and electronic media
2001
Brazil expands tobacco packaging rules to include health warnings and graphic images
2002
Brazil’s public health system begins offering free smoking cessation treatment
2006
Brazil joins the WHO Framework Convention on Tobacco Control, committing to global measures to reduce tobacco use and exposure
2007
Vital Strategies partners with Bloomberg Initiative to Reduce Tobacco Use in Brazil and 9 other countries
2009
ANVISA bans sale, import, and advertising of e-cigarettes; Brazil launches public campaigns to raise awareness about secondhand smoke
2011
Brazil implements its most comprehensive tobacco law, banning smoking in all indoor public spaces across the country and prohibiting cigarette advertisements
2012
Brazil introduces a cigarette excise tax with annual increases and becomes the first country to ban flavor additives in all tobacco products
2015
ANVISA develops smoking inspection training modules for better enforcement
2019
Brazil’s Attorney General sues major tobacco companies for industry misconduct and marketing to children
2024
The National Congress approves a selective tax reform on tobacco, soft drinks, and alcohol
Even with these successes, progress isn’t always linear. In 2023, Brazil saw its first significant increase in smoking prevalence in over three decades, due in part to political shifts and aggressive industry interference and marketing. These competing interests can undermine hard-won advances. Brazil’s successful campaign for front-of-package warning labels on unhealthy foods offers another example of progress, but like tobacco control, the gains rely on sustained, long-term action and enforcement, especially as growing threats continue to drive cancer risk further upwards.
Future Projections
On the Horizon for Brazil
Premature cancer mortality—deaths occurring before age 70—is projected to rise in Brazil over the coming decades. By 2050, the rate may increase by nearly 20%, from approximately 77 to 93 deaths per 100,000 people. When accounting for deaths at older ages, the cumulative toll is expected to reach 11 to 14 million cancer deaths over the next 25 years.
Premature cancer deaths will claim
4.8 million
Brazilian lives by 2050
These projections underscore both the scale of Brazil’s public health challenge and the opportunity for prevention. Despite the rising toll, Brazil has made measurable progress in reducing its overall cancer burden—particularly through tobacco control and early detection. These successes show that coordinated, evidence-based strategies can drive meaningful change. With strong data, clear communication, sound policies, and effective implementation, Brazil has the tools it needs to build on this progress and save millions of lives.
Of the projected 11-14 million cancer deaths by 2050, over 415,000 are expected to be caused by alcohol. Like tobacco-related cancers, these deaths are largely preventable. Comprehensive strategies—such as those used in tobacco control—are now urgently needed in other high-risk areas, including alcohol policy, where similar coordinated campaigns could have a powerful impact.
Alcohol Interactive
One Less Drink a Day Could Prevent Over 155,000 Cancer Deaths Over the Next 25 Years
The connection of alcohol consumption with the risk of death due to different types of cancers is quantifiable and well-established. By combining this evidence with data on alcohol consumption among the Brazilian population and projected cancer deaths in Brazil, we can estimate how many lives we could save through reduced alcohol consumption.
0 cancer deaths could be prevented by 2050
If Brazilian drinkers reduced their alcohol consumption by one drink (12 grams)
415,853
Forecasted Cancer Deaths related to Alcohol Consumption by 2050
Total deaths prevented by Cancer Type
Colon and rectum cancer
0Esophagus cancer
0Lip and oral cavity cancer
0Breast cancer
0Other pharyngeal cancers
0Laryngeal cancer
0Liver cancer
0Nasopharyngeal cancer
0This simulation estimates the potential reduction in projected cancer mortality in Brazil under three scenarios of 12g less, 24g less and 36g less alcohol consumption per day. Using a comparative risk assessment approach across alcohol-related cancers (esophageal, liver, laryngeal, nasopharyngeal, other pharyngeal, breast, colorectal, and lip and oral cavity cancers), we calculate the population attributable fraction for the scenarios by integrating three key datasets: cancer-specific relative risks by alcohol consumption level (GBD), current Brazilian alcohol consumption patterns by age and gender (WHO), and future cancer mortality projections (Globocan: Cancer Tomorrow) by cancer type, age and gender. Results represent the estimated reduction in cancer assuming that the underlying relative risks of developing the different cancer types due to alcohol consumption stay constant over the period considered.
Based on methodology adapted from: Estimation of the direct and indirect costs attributable to alcohol consumption in Brazil (Vital Strategies, 2024)
Our efforts to address alcohol-related harm combine data-driven research, public engagement, and policy advocacy to drive meaningful change. Studies on public attitudes and the social and economic impact of alcohol have informed strategic communication efforts, including mass media campaigns, policy briefings, and multilingual resources.
Following the Brazilian government’s recent approval of a historic tax reform, including a selective tax on alcohol, tobacco, and soft drinks, we are working with partners to promote excise tax rates that align with public health goals. These developments reflect growing momentum for using fiscal policy as a tool of public health, and highlight the promise of sustainable financing in supporting long-term health resilience.
Vital Strategies continues to work with a broad range of stakeholders to take concrete steps toward reducing alcohol’s impact as a risk factor for cancer and other health threats.
Conclusion
A Healthier Future For All
Non-communicable diseases are the defining global health challenge of our time, responsible for over 75% of deaths worldwide. The human cost is immeasurable, and the economic consequences, encompassing healthcare expenses and lost productivity, are crippling, particularly for low- and middle-income countries. This burden is projected to grow unless decisive action is taken.
Fortunately, as we’ve learned in Brazil, concerted action across policy, practice, and people works. After years of sustained efforts to curb tobacco use, lung cancer deaths have begun to show the first signs of decline in Brazilian men. And the good news is we are making progress around the world, from Indonesia to Turkey to Nigeria. By tackling NCDs and their risk factors, we can avert 39 million deaths by 2030 and generate a staggering $2.7 trillion in net economic benefits globally.
“When we work together and push for solutions that are grounded in data, backed by evidence, and driven by equity, we will create healthier and more vital futures for populations worldwide.”
Mary-Ann Etiebet, M.D., President and CEO, Vital Strategies
At Vital Strategies, we are committed to advancing health equity and building stronger, more resilient public health systems for all. This is how we protect lives, cut long-term costs, and ensure people everywhere have the chance to live their healthiest most fulfilling lives. Confronting the Global Cancer Crisis was built in partnership with Citizen Codex, a creative data studio that builds digital products that inspire change.
Partner with Us
We partner with governments, change makers, and researchers to move policy and people toward sustainable progress in global health.
Learn More
about partnerships